Share this
Top 3 Causes of Respiratory Problems in Nursing Homes
by HEPACART on Feb 07, 2020
Long-term care facilities have much in common with other healthcare facilities, especially infection control.
Like hospitals, nursing homes house infection-prone residents that share sources of air, food, and water in a crowded institutional setting.
But nursing homes differ in having a population that is generally more susceptible to infection and fatal outcomes, given the weaker immune systems and nearly universal presence of chronic illness among the elderly.
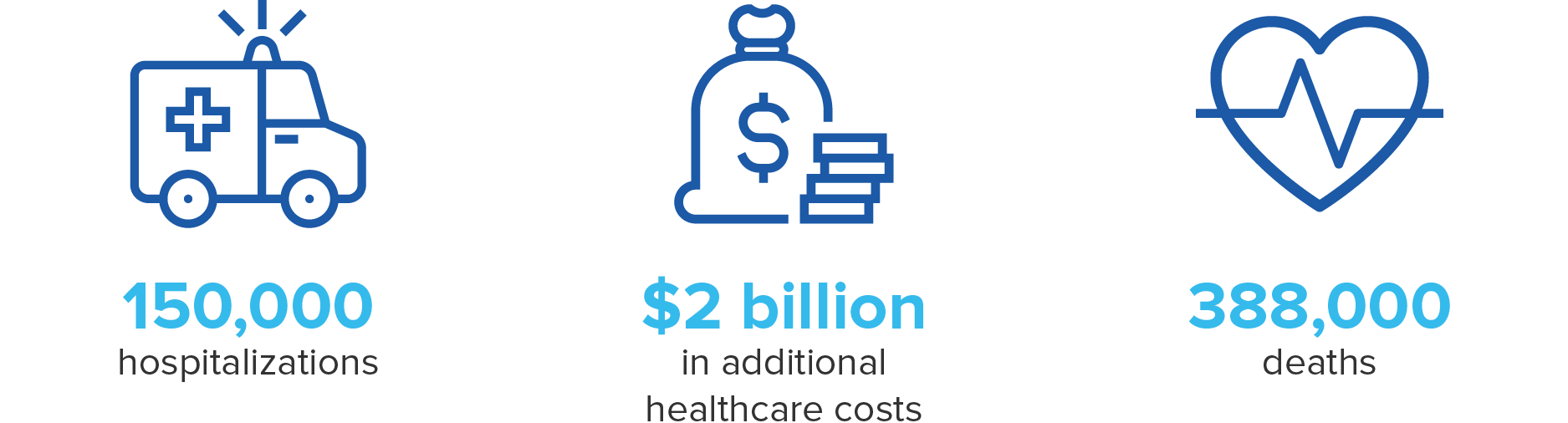
A 2011 study estimated there are between 1.6 and 3.8 million HAIs in nursing homes per year, resulting in 150,000 hospitalizations, 388,000 deaths, and up to $2 billion in additional healthcare costs.
Not surprisingly, infection prevention and control were identified as a priority under proposed rules for nursing homes by the Department of Health and Human Services in 2015, in which each facility would be required to have an infection prevention and control program and an infection prevention and control officer.
Unfortunately, many nursing homes are sub-par when it comes to protecting residents from healthcare-associated infections (HAI). Fifteen percent of U.S. nursing homes receive deficiency citations yearly, according to a study referred to in the 2015 paper Understanding Infection Prevention and Control in Nursing Homes. Low staffing levels were associated with higher rates of infection.
Kinds of Nursing Home Infections
- According to Nursing Homes and Infection Control: The Most Common Infections, the most-reported infection in nursing homes is the urinary tract infection. While morbidity rates are relatively low compared with, say, pneumonia, they are still much higher in the elderly than in younger patients with UTIs. This is due to factors such as long-term catheterization and the presence of more types of urinary tract pathogens in older patients.
- Clostridium difficile infections, a very common cause of diarrhea in nursing homes, disproportionately cause death in patients over 65.
- Influenza is lethal to a large number of nursing home residents, despite vaccines being available.
- Pneumonia is the leading cause of death, with Streptococcus pneumoniae the most common pathogen.
- Mycobacterium tuberculosis
- Parainfluenza virus
- Respiratory syncytial virus
Let's take a look at how respiratory tract pathogens, in particular, are introduced and spread within a facility, and what steps might be taken to minimize the spread of infection.
Cause #1: Visitors, staff, and transfers
Respiratory tract infections can come from residents whose immune systems are weakened and cannot contain latent bacteria. Examples include reactivation of tuberculosis from nonresidents, staff, or visitors with an acute respiratory infection, or residents returning from a hospital stay and carrying HAIs.

Once loose in the facility, the pathogens spread by infectious agents such as large respiratory droplets, airborne droplet nuclei, or direct contact.
Solutions:
- Schedule staff training to encourage hand-washing and wearing protective masks.
- Hang signage to encourage visitors to use masks and use hand sanitizer stations.
- Mandate universal influenza vaccinations among staff and residents.
- Utilize technological solutions such as the Germbuster 5000 air scrubber, the HEPACART Airborne Pathogen Disinfection Module, and HVAC Germbuster to protect residents from airborne pathogens using HEPA filtration and far-UV light to remove and physically destroy microbes.
Cause #2: Antimicrobial-resistant bacteria
WebMD says one in four nursing home residents has antibiotic-resistant bacteria. That doesn't mean they're symptomatic, but once they're colonized, they can spread the germ to others, and if their immune system weakens, they can become sick.
Prolonged antibiotic use and frequent interpersonal contact in nursing homes encourages the growth and spread of superbugs within a facility. For that reason, they are more prevalent than in hospitals, according to the WebMD post.
Solutions:
- Try to discourage overprescribing of antibiotics, a primary cause of drug-resistant bacteria, particularly in the U.S.
- Improve interfacility communication to make sure transfer patients finish the full course of antibiotics.
- Take steps to encourage simple hand-washing, as mentioned above.
Cause #3: Pathogens in maintenance- and construction-related dust
With the explosion of and in-demand need for eldercare being driven by millions of aging baby boomers, building expansion is a fact of life at many nursing homes. Controlling airborne dust that transports pathogens is crucial since something as simple as disturbing a ceiling tile can cause mold spores to enter the air. These microscopic pathogens may be harmless to most of us but can be deadly when inhaled by frail, ill, or functionally impaired residents of nursing homes.
Solutions:
- Follow rigorous dust containment protocols as outlined in the infection control risk assessment (ICRA) matrix.
- Become familiar with dust containment technology (a good source of information is Dust Containment Units: The Complete Guide).
- Use a mobile containment cart such as DUSTBUGGY and dust-containing cabling access point (CAP) for ceiling access.
- Isolate a room temporarily with a reusable module such as the HEPACART AnteRoom.
- Separate a major construction project from resident areas with reusable barrier walls such as STARC Systems RealWall or LiteBarrier.
Conclusion
It is every bit as important to control infection in nursing homes as in hospitals — perhaps even more so since nursing homes are both treatment centers and a permanent home for infection-prone residents who eat together and interact socially.
Explore all our infection control solutions to understand how technology, when used as an integral part of carefully managed infection control protocol, can help make long-term care facilities safer for everyone.
Resources
- The Importance of Dust Containment in Long-Term Care Facilities.
- Nursing Homes and Infection Control: The Most Common Infections
- Infectious Disease Outbreaks in Nursing Homes: An Unappreciated Hazard for Frail Elderly Persons
- Understanding infection prevention and control in nursing homes: A qualitative study.
- National Action Plan to Prevent Healthcare-Associated Infections
- Infectious Disease Outbreaks in Nursing Homes: An Unappreciated Hazard for Frail Elderly Persons
- Dust Containment Units: The Complete Guide


