Share this
How Dust, Mold, & Bacteria Wreak Havoc in Assisted Living Facilities
by HEPACART on Apr 21, 2021
Air quality is a priority to facilities management professionals who are responsible for the health of residents.
As we all know, the elderly are more susceptible to becoming ill from airborne pollen, dander, dust, mold, and bacteria. Spring and autumn are notorious for increasing obnoxious plant pollen and disgusting molds such as Cladosporium and Aspergillus Penicillium. Exposure to these little darlings may cause discomfort or could result in secondary bacterial or viral infections.
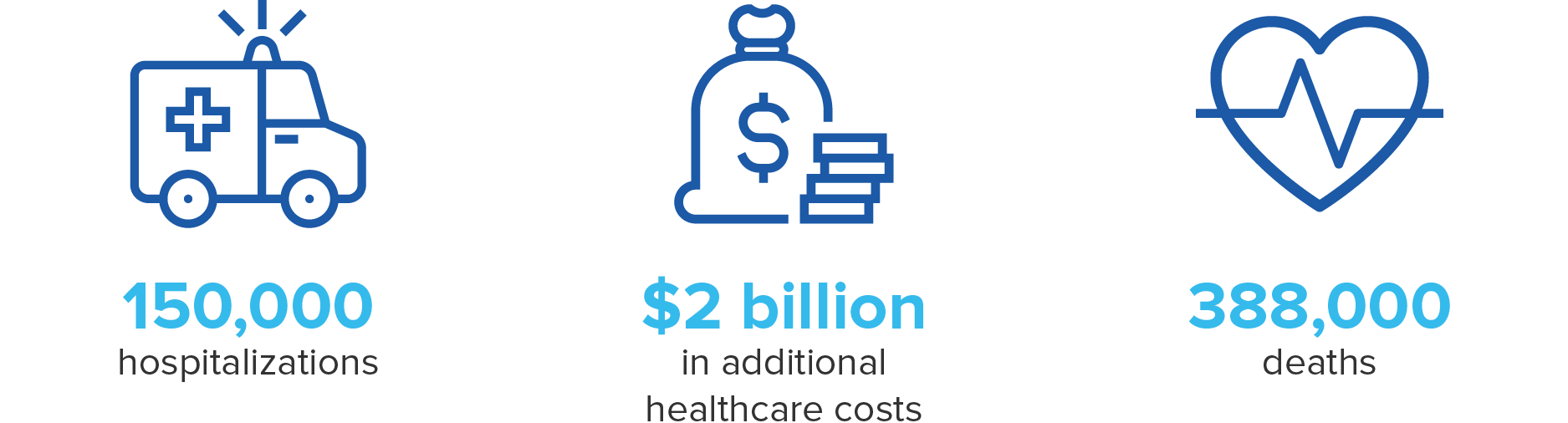
Yes, the change of seasons alone can contribute to a rise in healthcare-associated infections (HIAs) — which are always costly, sometimes deadly, and never mentioned in the same breath as having a good day.
Fortunately, you can learn how to identify environmental symptoms and take steps to prevent airborne dust, mold, bacteria, and viruses from ruining anyone's day. You can conduct regular building and room inspections, get rigorous about HVAC system maintenance, and place an air purifier in shared spaces.
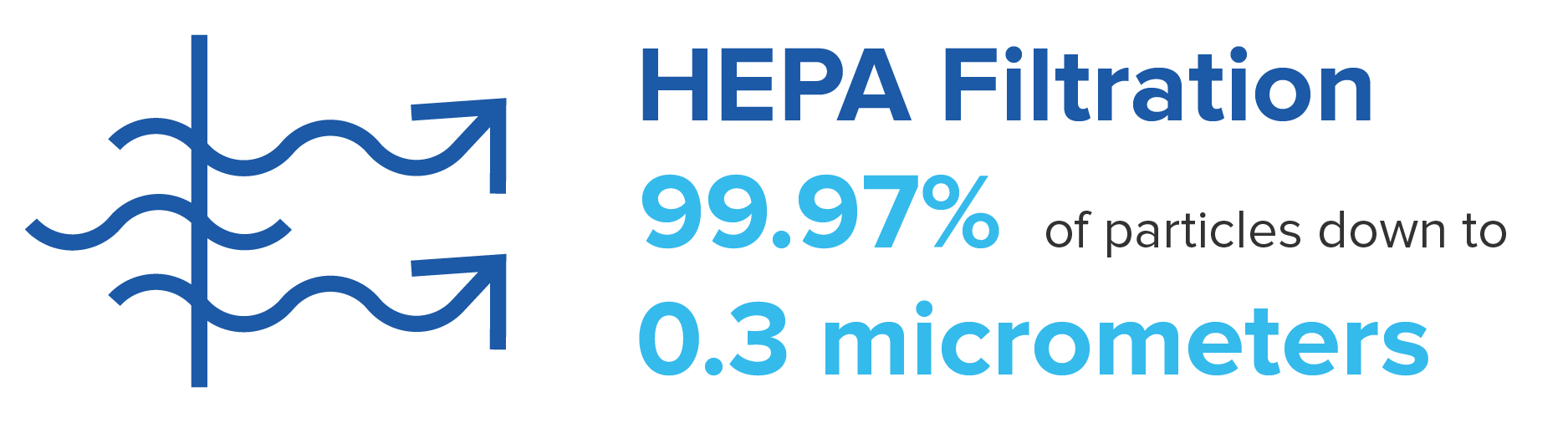
While we're on that subject, we recommend air purification systems equipped with HEPA filters that remove over 99% of harmful particles coupled with far-UVC light disinfection to destroy viruses. But we'll get into that in more detail at the end of this post.
What is poor air quality?
It's easy to get grossed out if you go looking for lists of all possible indoor air contaminants. So here's a brief overview.
- Humidity - from human exhaling, faucets, showers, water leaks, and outside air.
- Carbon dioxide - exhaled breath from occupants, staff, and visitors.
- Formaldehyde - fumes from adhesives, fabrics, stains, varnishes
- Volatile organic compounds (VOCs) - toxic gases and vapors from solvents, paints, etc.
- Molds, fungi - from stagnant water, drains, HVAC condensate pans, water leaks
- Bacteria, viruses - from coughing and sneezing occupants, staff, and visitors
- Dust mites - from carpets, furniture, bedding
- Dust - from construction or maintenance activities.
- Phthalates - off-gassing from adhesives, flooring, finishes, plumbing pipes
It doesn't take much for pollutants to reach lethal concentration for vulnerable residents: perhaps just a little bad luck mixed with some laissez-faire building maintenance, and before long, your facility starts to look like HAI Central. Of all the airborne pollutants listed, molds, fungi, bacteria, and viruses are among those most likely to be lethal to nursing home residents, so we'll now take a closer look at those.
Mold
How high is the risk from mold? This list from our December 2019 post about mold abatement shows some real-world consequences of mold growing unabated in healthcare facilities.
- 2017 - Mold at Two Pittsburgh Hospitals Linked to 5 Deaths
- 2017 - UPMC Sued by Family of Patient Who Died After Mold Infection
- 2019 - Dozens of Nurses and Staff Sickened by Mold in NYC Hospital
- 2019 - 1 Killed, 5 Infected by Mold at Seattle Children's Hospital
The main causes of mold in healthcare facilities are:
- Flooding
- Plumbing leaks
- Roof, wall, or window leaks
- Poorly designed HVAC systems
Once you have determined the cause of your mold problem, your first task is to track down sources of moisture, fixing leaks where necessary. You may need to call on HVAC experts to check your system's design and eliminate the root causes of moldy drip pans or drippy ductwork.
Second, determine how far and wide the mold has spread. You may need to relocate patients before proceeding to contain the affected area with portable wall barriers and anterooms. Then, control airflow using HEPA filter-equipped negative air machines to prevent the further spread of mold spores. This is extremely effective because HEPA filters remove over 99% of particles 0.3 micrometers or larger, and the smallest mold spores are about 4.0 micrometers in size.
Third, with containment and air management in place, cleaning and removal can begin. Mold-contaminated furniture, carpet, even walls must go, in some cases. You may want to leave the job to experts in mold abatement, who also will remove contaminated medical supplies. After cleaning with HEPA vacuums, disinfection begins. Remediation experts sometimes test using biological indicators, which are known, hardy spores sprinkled on surfaces to test the efficacy of disinfectants. If the known spores are killed, then other, less robust spores will have been eliminated too.
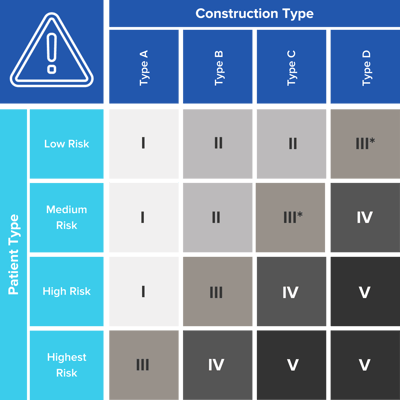
Dust
Your primary sources of hazardous dust will be from either maintenance or construction, and you'll need an infection control risk assessment to determine appropriate precautions. Guided by the ICRA Matrix, your infection control team will put together a plan to protect building occupants that includes containment. Dust containment is at the heart of what we do at HEPACART, supplying both equipment and information to support your infection control team's planning.
If construction dust is your main concern, be sure to read our post dedicated to that topic, How to Keep Air Clean in Healthcare Facilities During Construction, summarized here:
- Follow the ICRA matrix to determine myriad things such as relocating patients most susceptible to infection, temporary modifications to air handling and ventilation, and water system safeguards against opportunistic pathogens.
- Make sure your current HVAC system is up to spec in such areas as filters with high efficiency, condensation drainage, sufficient ventilation (mixing of outside air), and humidity control.
- Choose equipment that will cover all ICRA matrix classes, including Class IV. That provides maximum versatility by covering any maintenance or construction activities that fall into Classes I, II, or III.
Bacteria and viruses
With most seniors at nursing homes having been vaccinated against the SARS-CoV-2 virus that causes COVID-19, deaths from this terrible disease are down sharply. But there's still plenty of reason to disinfect the air in healthcare settings.
In a literature review of 206 infection outbreaks in nursing homes, 45% involved the respiratory tract, with influenza virus A or B and mycobacterium tuberculosis being primary pathogens.
An effective way to provide disinfection air in healthcare settings is to deploy equipment that uses far-UVC light. This technology is designed to neutralize viral and bacterial pathogens that are light enough to remain airborne for long periods and small enough to slip through HEPA filters.

You can roll a stand-alone room air purifier to areas where there are pockets of poor circulation, protecting residents in public or private rooms. Or you can add an airborne disinfection module to a negative air machine as another way to clean the air with far-UVC disinfection.
To read more on this topic, see our post Why Senior Living Facilities Directors Are Creating Disinfection Plans That Incorporate Far-UVC Light.
And that brings us from our damp and moldy introduction to a clean, germ-free conclusion because now you've seen the light — and it is far-UVC.
Resources

