Share this
ULPA VS. HEPA Filter: What's the Difference & Why Does It Matter?
by HEPACART on Mar 19, 2020
Understand when and why to choose HEPA or ULPA.
The HEPA filter gets mentioned frequently in this blog because it's effective technology that is central to HEPACART’s® mission: protecting patients from dust and pathogens in hospitals and other hazardous environments.
While all HEPA filters (High-Efficiency Particulate Air) meet ASME and DOE standards of 99.97%, some are more efficient. For instance, our HEPAFORCE® Negative Air Machines function at 99.99% efficiency. We call this "medical-grade" HEPA filtration.
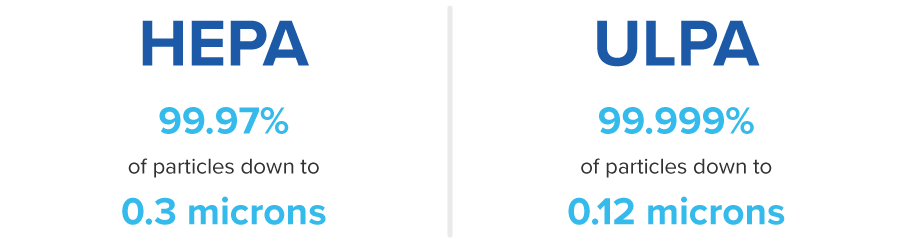
You may be aware that there's a filter that removes even smaller particles, called the ULPA (Ultra-Low Particulate Air) filter. The ULPA standard requires removal of 99.999% of particles down to 0.12 microns. That sounds much more effective than HEPA, so a legitimate question arises: When comparing ULPA vs. HEPA filters, why stick with HEPA?
In the words of Ricky Ricardo, we got some 'splainin' to do.
How Does Filtration Work?
First, let's take a detour to understand the behavior of particles moving through air filters. Both HEPA and ULPA filters consist of innumerable tiny strands of randomly arranged borosilicate glass microfibers.
Flowing through this vast labyrinth of fibers, particles get arrested through various physical mechanisms, the main three being interception, inertial impaction, and diffusion.
Interception occurs when the airstream carries a particle close enough to a fiber to stick to it.
Inertial impaction happens to larger particles that are too heavy to continue following the airstream as it flows around the fibers, so they collide with them and stick to them.
Diffusion describes the movement of the tiniest particles (below 0.1 micrometers) as they get knocked around by the Brownian motion of gas molecules in the air. Their erratic, zigzag path makes it more likely that they will collide with fibers.
Far from acting as a simple sieve, then, a fibrous air filter actually defies common sense by trapping smaller and larger particles more effectively than midsize particles. The worst-case particle size happens to be 0.3 micrometers, and that fact helped drive the design parameters of the HEPA filter.
ULPA vs. HEPA Filter Systems
OK, but if ULPA is better than HEPA at capturing more and smaller particles (such as tiny viruses), why are we still using HEPA?
It's because, in this case, "better" is only true in a narrowly-defined sense. While ULPA filters collect more particles in that hard-to-trap 0.12-0.4 range, they are only necessary for specialized applications such as microelectronics manufacturing or medical laboratories, removing particulates from cleanrooms, or filtering toxic surgical plumes emitted during electro-surgical operations.
HEPA filters, by contrast, are much more broadly used because they're considered optimal for most biological applications, including healthcare. As an example of why HEPA filters work so well in hospitals, consider that viruses, which are smaller than 0.3 micrometers and theoretically could pass through a HEPA filter, most often travel on larger particles such as saliva or sweat, thereby being trapped.
In short, here are some disadvantages that come with using ULPA filters.

Restricted Airflow: The main reason why you can't just swap in a ULPA filter for a HEPA filter is that the ULPA filter is more restrictive. As we discussed in this blog several years ago, a key difference between HEPA and ULPA is airflow. The denser media of the ULPA filter reduces airflow 20% to 50% for filters of the same dimensions. This greater pressure drop would lower a key metric, air changes per hour (ACH), to an unacceptably low level, resulting in worse air quality in a room.
Higher Cost: Since ULPA filters have denser media and are harder to produce than HEPA filters, they cost approximately 35 percent more than HEPA filters. And the cost of filters is only part of the story. Designing a ULPA system to deliver the same ACH as a HEPA system would require a larger filter to make up for the more restrictive flow, and possibly a more powerful blower, making the entire filter system larger and more expensive.
Shorter Life: Another thing that makes ULPA filters more costly is their shorter life, which averages five to eight years, compared to about 10 for HEPA filters in similar use. Also pre-filters are often used to protect the finer filters downstream, so additional pre-filtration could be necessary to protect the ULPA filter.
Conclusion
While at first, it may seem as if simply replacing your HEPA filter with a ULPA filter is a good idea, we hope you now understand why that wouldn't work. A filtration system designed for a certain airflow must be designed to anticipate the filter element's resistance to flow, and a ULPA filter would be too restrictive in a system designed for HEPA. More important is that ULPA filtration would be expensive overkill if substituted for HEPA in most applications.
Too often, procedures fail even when the right equipment is used. So what's most important is following the infection control precautions outlined in the ICRA Matrix, such as properly installing temporary barriers, creating a negative air environment with HEPA-equipped filtration machines, and cleaning with HEPA filtered vacuums.
For those charged with minimizing airborne dust and pathogens during construction in healthcare settings, HEPA filters are still the recommended standard. To get additional perspective, download our ULPA vs. HEPA Guide.
Additional resources